Health care has always been considered a recession-resistant industry. But when there’s a market downturn and employers cut staff, consumers tighten their belts everywhere — including their employer-funded telehealth perks, meditation app subscriptions or, if they’re unemployed, even seeing a doctor.
Many are also joining federal and state health insurance programs like Medicare, Medi-Cal and Medicaid. And venture firms and startups are taking notice: New health care startups that once vied for the eyes of employers and insurance companies are now targeting these patients.
Enter Author Health, a health care platform for Medicare Advantage recipients. The company launched on Wednesday armed with $115 million in financing from General Atlantic and Flare Capital Partners.
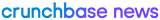
Search less. Close more.
Grow your revenue with all-in-one prospecting solutions powered by the leader in private-company data.
The Boston-based startup creates a team of doctors, nurses, therapists and community health workers for Medicare Advantage recipients with serious mental health disorders. Data from The Commonwealth Fund shows 1 in 4 people with Medicare — those in the U.S. who are age 65 and older, or those with a disability — have a mental illness, but only 40% to 50% receive treatment.
“They end up in inpatient units and emergency departments,” said Dr. Katherine Hobbs, CEO of Author Health. “A lot of that utilization and bad outcomes could be avoided by better care in the community in the outpatient setting.”
Bullish on federal health plans
Given medical advancements, there are more older people in the U.S. today than ever. As of 2022, there are more than 58.6 million people enrolled in Medicare.
So much health care spending has been funneled into government programs that startups are beginning to tap into it. EasyHealth, which raised $135 million in 2021 (per Crunchbase data), acts almost as an insurance brokerage that connects patients with different Medicare plans. Cityblock Health, provider of medical and behavioral care to Medicaid are patients, raised $400 million, also in 2021. Nashville, Tennessee-based CareBridge raised $140 million in 2022 to offer at-home care for state Medicaid beneficiaries. And retirement benefits startup Spark Advisors has raised $13.6 million over the past few years to branch into Medicare.
“Investors recognize the substantial need and also the opportunity that really will only continue to grow as the Medicare population grows,” Hobbs said.
Even Maven Clinic, the fertility platform that launched a direct-to-employer model, raised $90 million in 2022 to tap into Medicaid patient rolls.
“Medicaid is a priority for us. Nearly half of all the babies born in America are born into a Medicaid plan,” Will Porteous, Maven’s chief growth officer, told me last year. “There’s the opportunity to address over half of the babies born in the country, but then, too, oftentimes these are the most underserved communities in the country.”
There’s a catch — companies interested in tapping into Medicare and Medicaid beneficiaries have to prove their plans work. Employers are more likely to offer health care-related perks based on how they affect productivity, retention and happiness.
But startups looking to work with insurance providers have a higher bar to meet to prove their work lowers health care spend over time.
“There’s been a lot of investment over the last five years in behavioral health. Most of that investment has gone to mild to moderate conditions,” Hobbs said. “There’s really been very little investment around serious mental illness and substance use disorders.”
Correction: A previous version of this article incorrectly stated Cityblock Health worked with Medicare patients, not Medicaid patients. The post has been updated.
Illustration: Dom Guzman
Stay up to date with recent funding rounds, acquisitions, and more with the Crunchbase Daily.






![Illustration of 50+ woman on smartphone. [Dom Guzman]](https://news.crunchbase.com/wp-content/uploads/2021/01/Femtech_-300x168.jpg)

![Illustration of pandemic pet pampering. [Dom Guzman]](https://news.crunchbase.com/wp-content/uploads/2021/03/Pets-2-300x168.jpg)
67.1K Followers